It was shift change when the patient told his nurse that he had a terrible headache. It was unlike anything he’d ever felt before; a 10/10 on the pain scale. His nurse scanned the MAR and administered Tylenol 650 mg. No relief. The doctor was paged, and a STAT CT of the head was ordered. Within an hour, the unit phone rang, and the ID read RADIOLOGY. That isn’t good; the radiologists only call the unit if something critical is found that needs immediate response. It was an acute brain bleed and the patient needed to be evaluated by a neurosurgeon for possible surgical intervention. This hospital didn’t have neurology or neurosurgery services, so it became clear that an emergent transfer for higher level of care needed to take place. The unit secretary jumped on the task right away and called two nearby trauma centers. She sent copies of the patient’s medical records and explained the reason for the transfer. Both hospitals claimed they would review the chart and call back when they could assign a bed for this patient. Hours passed and there was still no accepting doctor, no bed assignment, no transport crew, and no relief for the patient. The night shift concluded, and the day team arrived to assume care.
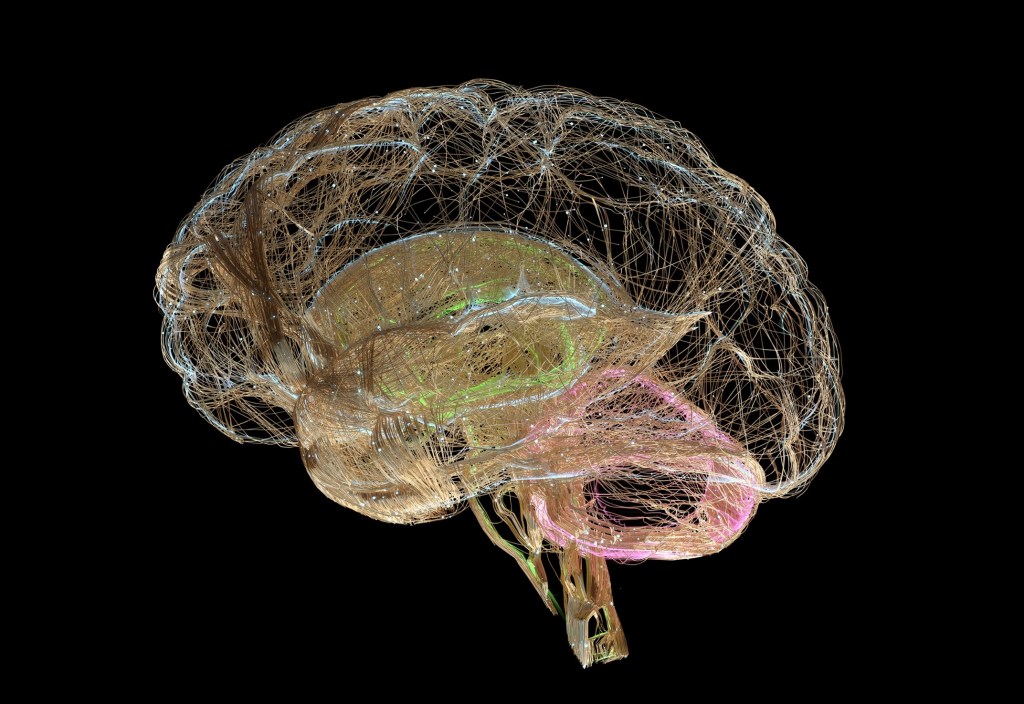
Why this is a problem: A hemorrhagic stroke or “brain bleed” is an absolute emergency. The brain is extremely sensitive to changes in pressure and an acute bleed can permanently damage brain cells. This patient could suffer lifelong injuries or even die. The unit secretary is a valuable member of the department’s team, but she is not clinical. She lacks the training, experience, and insight to understand and communicate the severity of this patient’s situation. There is a reason she couldn’t compel either hospital to accept the transfer immediately. Did she speak to the right person? Did she convey the severity of the situation? Then, instead of continuing to contact other hospitals, she alone decided that her two attempts were enough, and they would wait to get a response. ABSOLUTELY NOT. And by the way, why didn’t this patient’s primary RN advocate for expedited service? As each hour passed, the RN should have been asking for updates and escalating the issue up her chain of command.
Here’s what should have happened: The team gets word that this patient needs an immediate transfer for neurosurgery services. Either the primary RN or the provider should contact the RN House Supervisor with the need. The House Supervisor should call the House Supervisor of the potential receiving facility and communicate the circumstances. Paperwork is faxed over for the admitting provider to review and accept. The House Supervisor of the receiving facility assigns a bed and then transportation is arranged. I’ve seen this model work at other facilities and it is not only effective, but FAST. Let’s pack this guy up and get him to the chopper!
Leave a comment